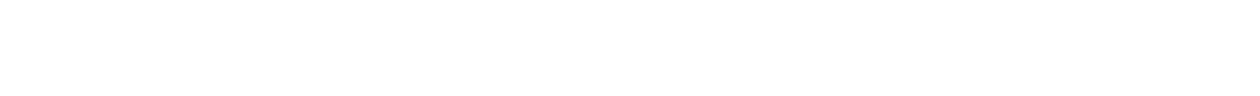
Aldosterone is a vital hormone that helps regulate blood pressure and electrolyte balance. Produced in the adrenal glands, aldosterone controls sodium and potassium levels, blood volume, and water retention. This hormone is critical for maintaining cardiovascular health and normal physiological function. However, abnormalities in aldosterone can lead to electrolyte imbalances and dysfunction in the kidneys, heart, and muscles. This article will provide an extensive overview of the definition, function, production, importance, effects, and risks of aldosterone.
What is Aldosterone?
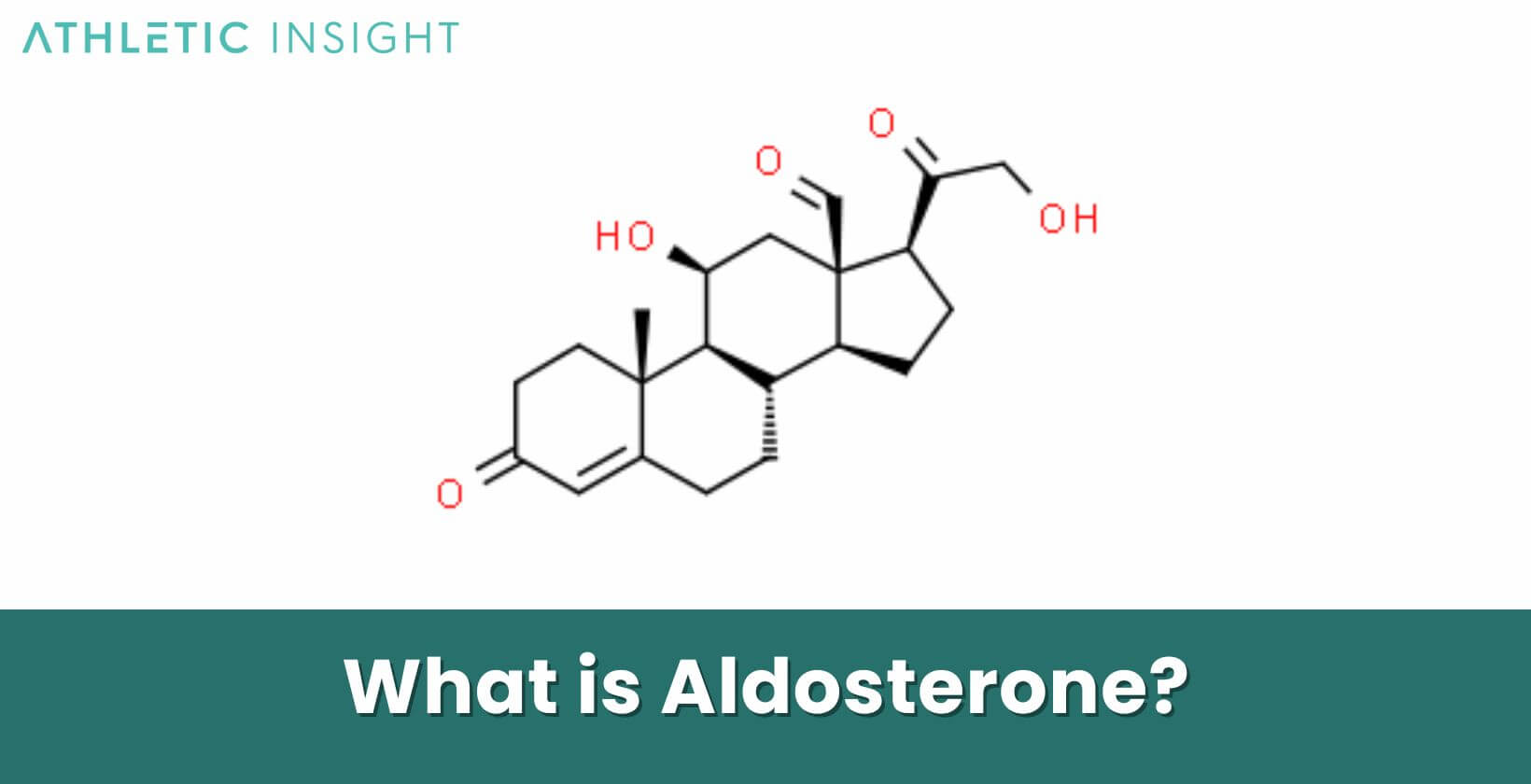
Aldosterone is a steroid hormone that is part of the renin-angiotensin-aldosterone system (RAAS). It is produced in the outer layer of the adrenal glands called the zona glomerulosa. Aldosterone is formed when the enzyme aldosterone synthase converts corticosterone into aldosterone. This mineralocorticoid hormone plays a major role in sodium retention, potassium excretion, and regulating blood pressure and blood volume.
The main trigger for aldosterone release is angiotensin II, a peptide hormone that signals the adrenal glands when blood pressure or blood volume is too low. This causes the adrenal cortex to synthesize and secrete aldosterone to increase these levels back to normal.
Once released into the circulation, aldosterone travels to its primary target organs – the kidneys and colon. In the kidneys, it acts on nephrons by stimulating the reabsorption of sodium ions and the excretion of potassium ions into urine.
Aldosterone increases the number of sodium-potassium pumps and sodium channels in the collecting ducts and late distal tubule of nephrons. This mechanism allows more sodium to be reabsorbed from the forming urine back into the blood while secreting more potassium. In the colon, aldosterone stimulates the reabsorption of sodium and associated water, which also increases blood volume.
What is the difference between Aldosterone vs ADHD?
Aldosterone is a hormone produced by the adrenal glands, responsible for regulating sodium and potassium balance in the body, which in turn affects blood pressure. It operates primarily through the renin-angiotensin-aldosterone system, acting on kidney cells to modulate the reabsorption of sodium and the excretion of potassium. Disorders related to aldosterone, such as primary aldosteronism, can lead to high blood pressure and other symptoms.
ADHD, or Attention Deficit Hyperactivity Disorder, is a neurodevelopmental disorder characterized by persistent patterns of inattention, hyperactivity, and impulsivity. Commonly diagnosed in childhood, ADHD symptoms can include difficulty staying focused, excessive talking, and impulsivity. It’s believed to arise from a combination of genetic, environmental, and neurological factors and is managed with behavioral therapy and medications.
What is the Function of Aldosterone?
The main function of aldosterone is to regulate blood pressure and intravascular volume by controlling the balance of electrolytes, primarily sodium and potassium. It carries out this key role by acting on the kidneys to increase reabsorption of sodium while excreting potassium out of the body. This leads to increased blood volume and pressure as more sodium and water is retained. Aldosterone coordinates this process by stimulating sodium transporters in the renal collecting ducts of the nephrons.
In conditions where blood pressure or volume drops too low, like dehydration, the RAAS is activated to secrete aldosterone. Aldosterone then signals the kidneys to reabsorb more sodium from the forming urine. The retention of sodium causes increased osmotic pressure, pulling water along with the sodium back into the blood. This expands the blood volume, leading to increased pressure. The concurrent excretion of potassium also helps regulatethe adrenal glands and blood pressure.
Does Aldosterone regulate blood pressure?
Yes, aldosterone is a key hormone involved in regulating blood pressure. It acts directly on the kidneys to increase blood volume and pressure through its effects on sodium reabsorption and potassium secretion. Aldosterone stimulates epithelial sodium channels and sodium-potassium ATPase transporters in kidney tubules. This facilitates the reabsorption of more sodium and water from the forming urine back into the bloodstream, increasing blood volume and pressure.
Additionally, aldosterone promotes the loss of potassium ions which has vasoconstrictive effects, leading to increased vascular resistance and blood pressure. Through these mechanisms, aldosterone maintains normal blood pressure levels. Excess aldosterone can cause hypertension, while aldosterone deficiency leads to hypotension and electrolyte disturbances.
What are the Best Supplements for Aldosterone?
If you’re looking for the best supplements related to aldosterone, you would need to find products related to hormonal balance, kidney function, and potentially blood pressure management. Aldosterone is a hormone produced by the adrenal glands. It helps regulate blood pressure by controlling sodium and potassium levels in the body.
For the best aldosterone supplements, you should consider and speak to your doctor about supplementing with potassium, magnesium, herbal supplements (ashwagandha, licorice root and holy basil), fish oil and Coenzyme Q10 (CoQ10). For the vast majority of people looking for a supplement for aldosterone, the best would be magnesium.
- Potassium Supplements: Since aldosterone regulates potassium levels, individuals looking to balance their aldosterone might be interested in managing their potassium levels. However, it’s essential to note that potassium supplements should be taken cautiously, as too much potassium can be harmful.
- Magnesium Supplements: Magnesium is another mineral that plays a role in maintaining proper blood pressure levels and may have a relationship with aldosterone function. It should be worth mentioning that magnesium supplements are popular and generally safe for most people.
- Herbal Supplements for Adrenal Support: Taking supplements like ashwagandha, licorice root, and holy basil may support adrenal gland health. Licorice root, in particular, can impact aldosterone levels but should be used cautiously as it can lead to adverse effects if taken in large quantities or for too long.
- Fish Oil/Omega-3 Fatty Acids: Omega-3 supplements can help support overall cardiovascular health and may indirectly relate to the hormonal balance and health areas impacted by aldosterone.
- Coenzyme Q10 (CoQ10): Coenzyme is an antioxidant that helps with blood pressure management and supports heart health, potentially benefiting those concerned with aldosterone levels.
What is the importance of Aldosterone in Nutrition?
Aldosterone plays an important role in nutritional balance through its regulation of electrolytes, especially sodium and potassium. These minerals are obtained through the diet and their levels must be maintained within narrow ranges for normal cellular function. Aldosterone stimulates the reabsorption of sodium from the kidneys back into the bloodstream. This allows the body to retain sufficient sodium obtained through food and prevent sodium depletion.
Aldosterone also promotes potassium excretion in the urine. Potassium is an abundant mineral in foods like fruits, vegetables, beans and dairy. The kidneys must excrete excess potassium consumed to prevent dangerous elevations in serum potassium. Aldosterone facilitates this regulation. A nutritional imbalance in sodium and potassium can disrupt aldosterone and have major impacts on blood pressure. Additionally, aldosterone affects fluid balance and kidney function which influence nutritional status.
How to control Aldosterone level?
There are several strategies that can help maintain healthy aldosterone levels within the normal range. Restricting sodium intake is important, as excess sodium consumption can increase aldosterone production. Eating foods higher in potassium, like bananas, spinach and potatoes can help reduce aldosterone secretion. Staying well-hydrated allows aldosterone levels to stabilize at an appropriate range.

Certain medications can also lower aldosterone, including angiotensin converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), and mineralocorticoid receptor antagonists like spironolactone. Improving overall lifestyle by losing excess weight, exercising regularly, limiting alcohol intake, and managing stress are also beneficial for controlling aldosterone.
What is the normal Aldosterone Level?
In healthy adults, typical aldosterone levels range from 3-16 ng/dL (nanograms per deciliter). Aldosterone levels are usually highest in the morning and decline later in the day. The normal range can vary based on testing methods. Levels outside of the expected range could indicate hyperaldosteronism, characterized by elevated aldosterone, or hypoaldosteronism, which is deficient aldosterone.
Maintaining aldosterone within the normal physiological range is important for electrolyte and fluid balance, kidney function, and cardiovascular health. Major deviations above or below this range can lead to dysfunction and adverse effects. Monitoring and regulating aldosterone is essential through proper diet, lifestyle, and medications when necessary.
What will happen if Aldosterone is too high?
Excessively high aldosterone levels, clinically known as hyperaldosteronism, can negatively impact health in several ways. It causes increased sodium and water retention, leading to elevated blood pressure and fluid accumulation. Hyperaldosteronism also leads to low serum potassium from increased urinary potassium wasting. This electrolyte imbalance can produce muscle cramps, weakness, and abnormal heart rhythms.
Chronically elevated aldosterone also promotes inflammatory and fibrotic changes in the kidneys and heart. This can accelerate damage and dysfunction. If severe aldosterone excess is left untreated, it can significantly increase the risk of cardiovascular disease, kidney failure, and even death. Therefore prompt diagnosis and treatment of hyperaldosteronism is crucial.
What will happen if Aldosterone is too low?
Deficient aldosterone levels, known clinically as hypoaldosteronism, can also have serious health consequences. With low aldosterone symptoms, the kidneys are unable to conserve sufficient sodium. This leads to excessive sodium and fluid loss in the urine, causing low blood volume and pressure. Hypoaldosteronism also reduces potassium excretion, leading to hyperkalemia.
The low blood pressure and reduced fluid levels from aldosterone deficiency can produce symptoms like fatigue, lightheadedness, and fainting. Low aldosterone also diminishes the kidneys’ concentrating ability, resulting in increased urination and risk of dehydration. If potassium builds up substantially from low aldosterone, it can cause dangerous heart arrhythmias. Prompt treatment is needed to resolve the electrolyte imbalances.
Does Aldosterone cause Electrolyte Imbalance?
Yes, abnormal aldosterone levels, both excessively high or low, can directly lead to electrolyte imbalance. Aldosterone regulates sodium and potassium homeostasis. In hyperaldosteronism, increased sodium reabsorption and potassium excretion cause low blood potassium. In hypoaldosteronism, there is excessive renal sodium wasting and potassium retention, leading to high blood potassium.
These electrolyte imbalances produce serious symptoms and effects on the cardiovascular system, muscles, and kidneys. Even minor fluctuations in aldosterone can alter electrolyte levels. Drastic changes increase the risk of dangerously high or low sodium and potassium. Monitoring and regulating aldosterone is key for preventing electrolyte disturbances.
How can Diet affect Aldosterone production?
Diet and nutrition significantly impact aldosterone synthesis and function. High dietary sodium intake is correlated with elevated aldosterone levels, as excess sodium ingestion triggers greater aldosterone release. Limiting foods high in salt can help reduce aldosterone production. In contrast, increasing dietary potassium, such as eating bananas, spinach, avocados, and potatoes, may lower aldosterone secretion.
Staying hydrated with adequate water intake also normalizes aldosterone by preventing dehydration and blood volume reductions. Excessive alcohol consumption can spur aldosterone release and lead to hypertension. Additionally, crash dieting or very low calorie intake stimulates aldosterone, so maintaining a balanced diet supports healthy levels.
How does Aldosterone affect Athlete performance?
Aldosterone assists athletic performance by maintaining fluid and electrolyte balance. Proper sodium levels enhanced by aldosterone are beneficial for hydration status. The potassium regulation aldosterone provides is also important, as potassium is vital for nerve transmission and muscle contraction during exercise.
However, very high aldosterone levels correlated with heavy sodium intake can potentially raise an athlete’s blood pressure. This may hinder performance. Optimizing aldosterone through diet and monitoring electrolytes is important for athletic performance, training and competition. Excessive training can also dysregulate aldosterone, so attention is required.
Do Athletes need to regulate their Aldosterone?
Yes, athletes should aim to maintain aldosterone within a healthy range for peak performance. The demands of intensive training and competition can affect aldosterone production and electrolyte balance. Monitoring sodium and potassium levels is helpful for athletes to detect imbalances early. Consuming proper amounts of electrolytes and staying hydrated assists with aldosterone regulation.
If excessive training is elevating aldosterone substantially, increasing potassium intake through diet and reducing sodium may help normalize levels. Seeking testing and medical guidance can also benefit athletes with dysregulated aldosterone. Overall, actively managing this key hormone is recommended for optimizing athletic ability and wellbeing.
Can Aldosterone be affected by exercise?
Yes, exercise and athletic training have significant effects on aldosterone secretion and balance. The physical stress of intense or prolonged exercise triggers the RAAS to release more aldosterone. This aims to maintain fluid levels and electrolyte concentrations which shift during exertion due to sweating and metabolic changes.
If exercise is extreme or exhaustion occurs, aldosterone levels may become excessively high post-workout. This can lead to fluid retention and hypertension. Proper rest, hydration, and moderating training helps normalize exercise-induced aldosterone spikes. Athletes should monitor sodium and potassium levels to detect imbalances from training. Overall, aldosterone is substantially influenced by physical activity.
What are the benefits of Aldosterone?
Aldosterone offers several benefits to the human body. Primarily, it ensures optimal fluid balance, enabling cells to function correctly and maintaining blood volume. By controlling the retention and excretion of sodium and potassium, it ensures these electrolytes remain at optimal levels for bodily processes.
Aldosterone also plays a role in sustaining blood pressure. Proper blood pressure is vital for the delivery of oxygen and nutrients to organs and tissues. Aldosterone’s role in regulating this is crucial for overall health.
- Maintains blood pressure within normal range
- Regulates sodium and potassium electrolyte balance
- Prevents low blood pressure and sodium depletion
- Allows kidney regulation of hydration and nutrients
- Promotes retention of appropriate fluid levels
- Prevents significant loss of ions in sweat during exercise
What are the risks of Aldosterone?
While aldosterone is essential for various physiological functions, imbalances can pose risks. Elevated aldosterone levels can lead to conditions like primary hyperaldosteronism, resulting in high blood pressure, heart issues, and kidney damage over time.
On the other hand, decreased aldosterone levels can cause hypoaldosteronism. This condition might lead to symptoms like muscle cramps, dizziness, and severe cardiac complications due to elevated potassium levels. Monitoring and regulating aldosterone is critical to avoid these potential risks.
- Hypertension from excess sodium retention
- Hypokalemia and hyperkalemia from imbalances
- Kidney damage from hyperfiltration
- Cardiac dysfunction and arrhythmias
- Muscle cramping and weakness
- Fluid retention and edema
- Dehydration from polyuria
- Exacerbation of chronic diseases